Assessment |
Biopsychology |
Comparative |
Cognitive |
Developmental |
Language |
Individual differences |
Personality |
Philosophy |
Social |
Methods |
Statistics |
Clinical |
Educational |
Industrial |
Professional items |
World psychology |
Cognitive Psychology: Attention · Decision making · Learning · Judgement · Memory · Motivation · Perception · Reasoning · Thinking - Cognitive processes Cognition - Outline Index
Vision Restoration Therapy (VRT) is a noninvasive, nonsurgical form of Vision therapy provided by NovaVision.[1] This therapy was developed by Bernhard Sabel, Ph.D. The phenomenon underlying the therapy is visual neuroplasticity.[2]
Description of therapy[]
Vision Restoration Therapy is a computer-based treatment therapy, and is used to help patients with visual field defects regain function by stimulating existing visual neurons to rewire and make new connections.[3] This therapy is cleared by the U.S. Food and Drug Administration (FDA) to treat visual field defects due to stroke, head injury, brain tumors, and brain surgery. Some other defects that can also be treated with VRT include hemianopia, quadrantanopia, scotoma, and diffuse field defect.[2]
Criteria to undergo therapy[]
To have the greatest chance of possible recovery, patients must first go through screening criteria with their physicians to see if they can effectively undergo VRT. A few of the major criteria are listed below.
- Patients that have photosensitive epilepsy, serious eye disease, or prominent cognitive deficits may not be eligible to undergo VRT treatment.
- An appropriate level of cognition is necessary due to the demand of great concentration and attention needed to pursue an effective treatment regimen.
- A minimum visual acuity of 20/200 is also required for proper stimuli detection.[2]
Advantages[]
Listed below are some of the advantages associated with VRT.
- The benefits of the therapy for a patient are not confined by the duration of time that the patient has had the visual defect. In other words, the benefits are not limited by the time difference between the time the patient developed the defect and the time of starting Vision Restoration Therapy.
- There is no age limitation for a patient to undergo treatment.
- The type of visual field defect does not limit the benefits of VRT.[2]
- There are no major side effects associated with VRT treatment. A few patients have reported mild infrequent headaches during treatment.[3]
Statistics[]
It is reported that about 70% of the patients that undergo the treatment have improvements in their visual fields. About 90% of the patients also stated that the use of the therapy has been accompanied by at least one major benefit. Some of these benefits include, improved reading, improved mobility, increased confidence, and independence. Around 88% of the patients also reported a better quality of life after completion of the therapy. Although results vary among patients, the therapy expands the visual field on average by 5°. This is associated with a 5° retraction in the blind field. The blind field is the antagonist of the visual field, and an expansion of the blind field is associated with visual field loss.[2]
Science behind the therapy[]
Neuroplasticity[]
The discovery of neuroplasticity has been hailed by some scientists to be one of the greatest discoveries ever. Neuroplasticity is the ability of the brain to adapt to the environment by making changes in itself over time. New technologies and therapies are being developed to harness the power of neuroplasticity in order to heal the repercussions of brain-related damage and injury. Vision Restoration Therapy is one such therapy that exploits visual neuroplasticity to alleviate visual field defects. VRT has been shown to expand the visual fields of patients and the repetitive activation and stimulation of functional neurons is the heart of the therapy.[4]
Harnessing the power of visual neuroplasticity for therapeutic purposes[]
Work in understanding visual neuroplasticity has made progress in the past decade. The potential for visual neuroplasticity can exist for a long duration of time. There are two approaches as of now to take advantage of this potential visual neuroplasticity.
- The first approach involves rescuing, regenerating, or transplanting visual neurons by biological/pharmacological methods. One example of this approach is the discovery of the regeneration of axons of retinal ganglion cells (RGCs) by introducing several proteins into the chemical environment of these cells. Some of these known proteins that induce axon growth of RGCs include laminin, Gap-43 protein, fatty acid binding protein, calmodulin, Alpha crystallin, IFN-gamma, cyclin-dependent kinase inhibitor protein, beta-hemoglobin, 60s-ribosomal protein, GAP-DH, and ADP-ribosylation factor.
- The second approach involves improving visual functions by stimulating the associated neurons in either the blind region of the visual field through different pathways or by stimulating damaged areas of the border region. This approach is a more promising approach than the first in harnessing visual neuroplasticity to help regain visual functions.[4] Vision Restoration Therapy is an example of this approach.
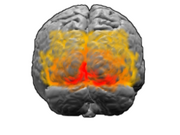
The Primary Visual Cortex (red) is shown along with the extrastriate visual cortical areas (orange and yellow) from the rear view. These areas make up the Visual Cortex.
Biology of visual neuroplasticity[]
An Illustration of the Visual System.
With visual neuroplasticity, reorganization of the physical structure of the brain occurs concurrently with reorganization of the visual system by new connections made by stimulated neurons. Using the imaging technique of fMRI, it was found that brain activity was altered after Vision Restoration Therapy. This associates cerebral reorganization with VRT treatment.[2][5]
The cerebrum is involved with higher brain function, and one component of the cerebrum is the primary visual cortex. The primary visual cortex is a region in the occipital lobe that can be altered by neuroplasticity to create new neuronal pathways around damaged areas to help regain lost visual functions. Sensory visual information is sent from the retina of the eye to the Lateral geniculate nucleus (LGN) in the Thalamus, which relays the visual information to the primary visual cortex by the fibers of the optic radiation. Lesions or damage to parts of the brain that cause visual field defects usually occur posterior to the optic chiasm.[6] Although the exact mechanisms that underlie regaining visual field functions through visual neuroplasticity and VRT are not yet fully known, the reorganization of the primary visual cortex is thought to make new connections and pathways in the optic radiation to the LGN to help regain visual field functions. The stimulation of existing neurons near a damaged site in the brain can form new synapses with other functional neurons to help take on and compensate for the function lost due to the damaged neurons. This is what is theorized to occur during VRT treatment.[6][2][4]
Vision Restoration Therapy stimulates the retina of the eye using repetitive points of light that flash on a computer screen. These flashing lights are aimed to stimulate the border of the blind area of a patient’s visual field. The repetitive stimulation is used to help promote visual neuroplasticity and ultimately make new neuronal connections to regain and expand the visual field.[2][4]
Process of therapy[]
Patients undergo therapy in the comforts of their home due to it being a software-based therapy sent to patients as a specialized portable apparatus called NovaVision VRT Device. The therapy requires a prescription from a physician in order to begin. A set of initial evaluation tests are taken using the VRT device to assess the amount of visual impairment and the locations of the borders of the visual field deficit. The therapy provider, NovaVision, then analyzes these data to customize the treatment to target these borders of deficit to help expand the visual field. Usually, patients complete the treatment course in 6 months. The therapy consists of patients using the VRT device for 30 minutes twice a day for 6 days of the week during the 6 month treatment course.[2]
Patients perform this therapy using the VRT device as stated before. The VRT device consists of a chin rest and a specialized computer screen that has High Resolution Perimetry (HRP) incorporated into its software. The built-in HRP helps in assessing and tracking the progress of the patient. The device sends this data directly to the therapy provider for feedback to modify the treatment if necessary.[2] HRP is used to map the visual field of a patient. This allows the therapy providers to have a representation of the patient's visual field.[7] For a general VRT session, the patient’s head is situated at eye level with the VRT device. The therapy begins by projecting a fixation point in the center of the screen. The patient focuses on this fixation point for the entire session. As the patient is focusing on the central fixation point, an individual point appears somewhere on the screen. Only one point is projected at a time alongside the fixation point. The patient must click the mouse every time he or she sees this point while focusing on the fixation point. These responses are collected to calculate stimuli detection rate and response time of the patient. In an effort to see the points on the screen most clearly, the therapy should be conducted in a dimly lit room.[2]
Skepticism[]
The effectiveness of VRT has been a controversial topic. Beneficial results have been researched and documented by testing small groups of patients. This has led to skepticism by some of the scientific community.[7] Even though VRT has been available for a few years now, optometrists, ophthalmologists, and other eye specialists do not regularly recommend VRT for their patients. The primary cause of this is that eye specialists rarely recommend this therapy to other eye specialists. The skepticism of VRT may be the source of the lack of recommendation.[8]
When VRT was first introduced, the primary skepticism involved the data collection methods that the VRT researchers used to quantify the effective results of using the therapy. The main argument was that the HRP data from the VRT device that was used to measure the progress of the patients was the same data used to show the effectiveness of VRT. These data would not be as reliable as data gathered using some other Perimetry technique.[9] Skeptics turned to studies that assessed VRT effectiveness using Tubinger Automatic Perimetry and Scanning laser ophthalmoscopy (SLO), which showed that no beneficial results in improving the visual field were associated with VRT use.[9] Skepticism also arose about the quality of life questionnaire surveys that patients took after VRT treatment. The possibility of the placebo effect could be present in the answering of these questionnaires.[9] Patients could have stated that their qualities of life did improve just because they had finished the therapy, even if no improvements actually occurred. Others questioned the neuroplastic mechanism behind VRT, stating that no salvageable tissue remains in the occipital lobe with vision deficits such as hemianopia. Neuroplasticity cannot make new connections according to this claim, which debunks VRT in its entirety.[9][10] It was proclaimed that eye movements were the cause of visual rehabilitation instead of self regeneration of the brain and visual neuroplasticity.[9]
Clinical studies and research[]
Much of the research that was initially conducted did not convince many of the scientific community that VRT is an effective treatment option for large scale use. As a result, many studies have been conducted to target the arguments of the skeptics.
Studies with large sample sizes[]
Much skepticism arose due to the fact that many of the initial studies of VRT effectiveness used only small sample sizes. One study aimed to show the effectiveness of VRT using a large sample size as a result. Researchers assessed the effectiveness of VRT by testing 302 patients. The study used the qualitative data from HRP, the stimulus detection rate, and the average response time before and after the patients underwent VRT. The stimulus detection rate did vary. About 38.3% of patients had great improvements, 32.6% had moderate improvement, and 29.1% had no improvement. The average reaction time also improved for the patients. It fell from 463.6 ± 5.08 ms to 446.2 ± 5.23 ms. This study showed that even assessing a large sample size yields the same positive results of effectiveness as the small sample size studies.[7]
Comparing perimetry techniques[]
The other criticism was that the perimetric data from the SLO showed that there was no improvement in the visual fields of patients that undergo VRT. Studies have compared and contrasted the various Perimetry techniques in Vision Restoration Therapy effectiveness. To reiterate, perimetry is visual field testing, and there are several perimetry techniques to measure visual fields. It was found that perimetric analysis using SLO was a more difficult task than commonly used Perimetry techniques such as HRP.[11] For comparison, SLO and HRP will be used as examples. SLO displays 3 black points on a bright red background, whereas HRP uses a bright red point on a black or grey background. The task of perceiving the black points on the red background in SLO was found to be a difficult task for patients with brain damage.[11] Also, the added attention needed to perceive all three points in SLO makes the task more difficult. Lastly, patients acknowledge that they see the points of light verbally in SLO. Patients just click the mouse after seeing a point in HRP. Verbal acknowledgement may reduce response time and seems an inefficient way to measure response time. These findings challenged the skeptics in relying on SLO data to measure the effectiveness of VRT.[12][11][13] A recent study assessed VRT effectiveness using fundus-controlled microperimetry to measure visual fields. The findings concluded that VRT was indeed effective in expanding the visual field. The microperimetry technique compensates for eye movements.[14]
Role of eye movements on visual rehabilitation[]
Studies were initiated to observe the role of eye movements as the reason behind visual field improvements. It has been debated that patients with visual field defects try to make up for their limited vision by making more frequent eye movements in an effort to expand their visual field. This theory debunks the efficacy of VRT and neuroplasticity as the cause of visual field expansion. Research has found that VRT does not change eye movements and the visual field improvements and expansion are independent of these movements.[15]
Long-term use and stability of VRT[]
Other studies have looked into long term use of VRT and the stability of visual field improvements after VRT treatment. One study looked into the effectiveness of VRT in improving visual fields by using the therapy for 12 months as opposed to the recommended 6 months. It was found that miniscule improvements occur after the first 6 month interval. The result also validate that treatment for 6 months is the optimal time for the therapy.[16] Another study looked into the stability of the results from VRT treatment. Patients were reassessed using Perimetry techniques about 2 years after they underwent VRT. The findings suggest that there is stability in the visual field improvements after VRT treatment. However, the stability is dependent on the patient to use the restored visual functions continuously and naturally to keep stimulating the new neuronal connections to achieve stronger visual functioning.[17]
Predictive outcome models of VRT effectiveness[]
Having a predictive model is beneficial for practitioners to get a general idea of the potential improvements by a certain procedure or treatment. Researchers have developed a Treatment Outcome Predictive Model to calculate the potential visual field recovery after VRT. This model uses several perimetric variables to make scientific predictions on a patient’s potential visual field recovery using VRT.[18]
Pilot studies[]
Pilot studies have also looked into the effects of Vision Restoration Therapy in treating visual field defects that have resulted from anterior ischemic optic neuropathy and glaucoma. Although these are pilot studies and require more data, it seems promising that VRT can help restore some visual functions of patients with anterior ischemic optic neuropathy.[19] The same promising results were found for patients with glaucoma. Some visual functions were able to be restored after VRT treatment.[20]
References[]
- ↑ Caplan, L. R., Firlik, A., Newman, N. J., Pless, M., Romano, J. G., & Schatz, N. (2005). Vision restoration therapy. [Letter]. British Journal of Ophthalmology, 89(9), 1229-1229. doi: 10.1136/bjo.2005.069773
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Frequently Asked Questions: Vision Restoration Therapy: Vision Rehab after Stroke or TBI. (2007). Retrieved November 12, 2010 from NovaVision, us.novavision.com: http://us.novavision.com/frequently-asked-questions.html
- ↑ 3.0 3.1 Romano, J. G., Schulz, P., Kenkel, S., & Todd, D. P. (2008). Visual field changes after a rehabilitation intervention: Vision restoration therapy. [Article]. Journal of the Neurological Sciences, 273(1-2), 70-74. doi: 10.1016/j.jns.2008.06.026
- ↑ 4.0 4.1 4.2 4.3 Sabel, B. A. (2008). Plasticity and restoration of vision after visual system damage: An update. [Article]. Restorative Neurology and Neuroscience, 26(4-5), 243-247.
- ↑ Vision Restoration Therapy Shown To Improve Brain Activity In Brain Injured Patients. (2007). Retrieved September 11, 2010 from ScienceDaily, www.sciencedaily.com: http://www.sciencedaily.com/releases/2007/08/ 070814082950.htm.
- ↑ 6.0 6.1 Farah, M. J. (2000). The Cognitive Neuroscience of Vision. Malden, Massachusetts: Blackwell Publishers Inc.
- ↑ 7.0 7.1 7.2 Mueller, I., Mast, H., & Sabel, B. A. (2007). Recovery of visual field defects: A large clinical observational study using vision restoration therapy. [Article]. Restorative Neurology and Neuroscience, 25(5-6), 563-572.
- ↑ Dr. Mona Patel, Doctor of Optometry at the Ochsner Clinic LLC in Marrero,LA. Interview date October 25, 2010.
- ↑ 9.0 9.1 9.2 9.3 9.4 Horton, J. C. (2005). Disappointing results from Nova Vision's visual restoration therapy. [Editorial Material]. British Journal of Ophthalmology, 89(1), 1-2. doi: 10.1136/bjo.2004.058214
- ↑ Disappointing results from Nova Vision’s visual restoration therapy
- ↑ 11.0 11.1 11.2 Sabel, B. A. (2005). Vision restoration therapy. British Journal of Ophthalmology, 89(5), 522-524. doi: 10.1136/bjo.2005.068163
- ↑ Kasten, E., Guenther, T., & Sabel, B. A. (2008). Inverse stimuli in perimetric performance reveal larger visual field defects: Implications for vision restoration. [Article]. Restorative Neurology and Neuroscience, 26(4-5), 355-364.
- ↑ Sabel, B. A., Kenkel, S., & Kasten, E. (2004). Vision restoration therapy (VRT) efficacy as assessed by comparative perimetric analysis and subjective questionnaires. [Article]. Restorative Neurology and Neuroscience, 22(6), 399-420.
- ↑ Marshall, R., Chmayssani, M., & O'Brien, K. (2010). Visaul field expansion after visual restoration therapy. [Article]. Clinical Rehabiliatation, 24, 1027-1035.
- ↑ Kasten, E., Bunzenthal, U., & Sabel, B. A. (2006). Visual field recovery after vision restoration therapy (VRT) is independent of eye movements: An eye tracker study. [Article]. Behavioural Brain Research, 175(1), 18-26. doi: 10.1016/j.bbr.2006.07.024
- ↑ Mueller, I., Gall, C., Kasten, E., & Sabel, B. A. (2008). Long-term learning of visual functions in patients after brain damage. [Article]. Behavioural Brain Research, 191(1), 32-42. doi: 10.1016/j.bbr.2008.03.005
- ↑ Kasten, E., Muller-Oehring, E., & Sabel, B. A. (2001). Stability of visual field enlargements following computer-based restitution training - Results of a follow-up. [Article]. Journal of Clinical and Experimental Neuropsychology, 23(3), 297-305.
- ↑ Guenther, T., Mueller, I., Preuss, M., Kruse, R., & Sabel, B. A. (2009). A Treatment Outcome Prediction Model of Visual Field Recovery Using Self-Organizing Maps. [Article]. Ieee Transactions on Biomedical Engineering, 56(3), 572-581. doi: 10.1109/tbme.2008.2009995
- ↑ Jung, C. S., Bruce, B., Newman, N. J., & Biousse, V. (2008). Visual function in anterior ischemic optic neuropathy: Effect of Vision Restoration Therapy - A pilot study. [Article]. Journal of the Neurological Sciences, 268(1-2), 145-149. doi: 10.1016/j.jns.2007.12.001
- ↑ Gudlin, J., Mueller, I., Thanos, S., & Sabel, B. A. (2008). Computer based vision restoration therapy in glaucoma patients: A small open pilot study. [Article]. Restorative Neurology and Neuroscience, 26(4-5), 403-412.
| This page uses Creative Commons Licensed content from Wikipedia (view authors). |