(took out notable case section) |
|||
| Line 76: | Line 76: | ||
== See also == |
== See also == |
||
| ⚫ | |||
| ⚫ | |||
*[[Edible salt]] |
*[[Edible salt]] |
||
| + | *[[Cerebral salt-wasting syndrome]] |
||
| ⚫ | |||
| ⚫ | |||
== Reference == |
== Reference == |
||
Latest revision as of 17:33, 4 November 2012
Assessment |
Biopsychology |
Comparative |
Cognitive |
Developmental |
Language |
Individual differences |
Personality |
Philosophy |
Social |
Methods |
Statistics |
Clinical |
Educational |
Industrial |
Professional items |
World psychology |
Biological: Behavioural genetics · Evolutionary psychology · Neuroanatomy · Neurochemistry · Neuroendocrinology · Neuroscience · Psychoneuroimmunology · Physiological Psychology · Psychopharmacology (Index, Outline)
Na-TableImage.png|
| ICD-10 | E871 | |
|---|---|---|
| ICD-9 | 276.1 | |
| OMIM | {{{OMIM}}} | |
| DiseasesDB | {{{DiseasesDB}}} | |
| MedlinePlus | {{{MedlinePlus}}} | |
| eMedicine | {{{eMedicineSubj}}}/{{{eMedicineTopic}}} | |
| MeSH | {{{MeshNumber}}} | |
The electrolyte disturbance hyponatremia (British hyponatraemia) exists in humans when the sodium (Natrium in Latin) concentration in the plasma falls below 135 mmol/L. At lower levels water intoxication may result, an urgently dangerous condition. Hyponatremia is an abnormality that can occur in isolation or, as most often is the case, as a complication of other medical illnesses. In the case of other mammals, particularly agricultural animals, different indications are relevant. The following refers to humans; an introduction to sodium deficiency in cattle is appended.
Symptoms
Most patients with chronic water intoxication are asymptomatic, but may have symptoms related to the underlying cause.
Severe hyponatremia may cause osmotic shift of water from the plasma into the brain cells. Typical symptoms include nausea, vomiting, headache and malaise. As the hyponatremia worsens, confusion, diminished reflexes, convulsions, stupor or coma may occur. Since nausea is, itself, a stimulus for the release of ADH, which promotes the retention of water, the potential for a vicious circle of hyponatremia and its symptoms exists.
Causes
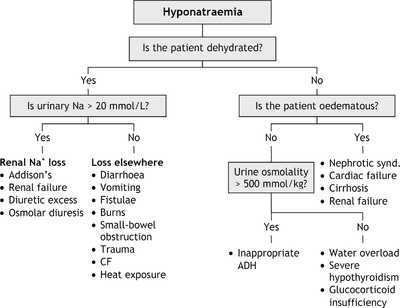
Causes of hyponatraemia
An abnormally low plasma sodium level is best considered in conjunction with the person's plasma osmolarity and extracellular fluid volume status.
Most cases of hyponatremia are associated with reduced plasma osmolarity. In fact, the vast majority of adult cases are due to increased vasopressin, i.e., anti-diuretic hormone (ADH). Vasopressin is a hormone that causes retention of water, but not salt. Hence, the patient with hyponatremia can be viewed as the patient with increased ADH activity. It is the physician's task to identify the cause of the increased ADH activity in each case.
In patients who are volume depleted, i.e., their blood volume is too low, ADH secretion is increased, since volume depletion is a potent stimulus for ADH secretion. As a result, the kidneys of such patients hold on to water and produce a very concentrated urine. Treatment is simple (if not without risk) — simply restore the patient's blood volume, thereby turning off the stimulus for ongoing ADH release and water retention.
Some patients with hyponatremia have normal blood volume. In those patients, the increased ADH activity and subsequent water retention may be due to "physiologic" causes of ADH release such as pain or nausea. Alternatively, they may have the Syndrome of Inappropriate ADH (SIADH). SIADH represents the sustained, non-physiologic release of ADH and most often occurs as a side effect of certain medicines, lung problems such as pneumonia or abscess, brain disease, or certain cancers (most often small cell lung carcinoma).
A third group of patients with hyponatremia are often said to be "hypervolemic". They are identified by the presence of peripheral edema. In fact, the term "hypervolemic" is misleading since their blood volume is actually low. The edema underscores the fact that fluid has left the circulation, i.e., the edema represents fluid that has exited the circulation and settled in dependent areas. Since such patients do, in fact, have reduced blood volume, and since reduced blood volume is a potent stimulus for ADH release, it is easy to see why they have retained water and become hyponatremic. Treatment of these patients involves treating the underlying disease that caused the fluid to leak out of the circulation in the first place. In many cases, this is easier said than done when one recognizes that the responsible underlying conditions are diseases such as liver cirrhosis or heart failure — conditions that are notoriously difficult to manage, let alone cure.
Hyponatremia can result from dysfunctions of the mineralocorticoid aldosterone (i.e. hypoaldosteronism) due to adrenal insufficiency, congenital adrenal hyperplasia, and some medications.
It is worth considering separately, the hyponatremia that occurs in the setting of diuretic use. Patients taking diuretic medications such as furosemide (Lasix), hydrochlorothiazide, chlorthalidone, etc., become volume depleted. That is to say that their diuretic medicine, by design, has caused their kidneys to produce more urine than they would otherwise make. This extra urine represents blood volume that is no longer there, that has been lost from the body. As a result, their blood volume is reduced. As mentioned above, lack of adequate blood volume is a potent stimulus for ADH secretion and thence water retention.
A recent surge in death from hyponatremia has been attributed to overintake of water while under the influence of MDMA. Also, Almond et al.[1] found hyponatremia in as many as 13% of runners in a recent Boston Marathon, with life-threatening hyponatremia (serum Na below 120 mmol/L) in 0.6%. The runners at greatest risk of serious water intoxication had moderate weight gain during the race due to excessive water consumption (see reference). Siegel et al [2] recently found that in addition to over-zealous drinking, the cause of exercise-associated hyponatremia (EAH)is from an inappropriate secretion of the hormone arginine vasopressin, or antidiuretic hormone. This excess hormone secretion prevents the kidneys from excreting the excess water in the urine.
Hyponatraemia is associated with both TCAs and SSRIs. It is more common in elderly people and in those taking diuretics. Consider hyponatraemia in all people who develop drowsiness, confusion, or convulsions while taking an antidepressant drugs.
Pseudohyponatremia
A normal or high plasma osmolarity with hyponatremia is called pseudohyponatremia. Pseudohyponatremia may be caused if extraordinarily high lipid or protein levels in the plasma interfere with the sodium assay.
Hypoosmolar hyponatremia
When the plasma osmolarity is low, the extracellular fluid volume status may be in one of three states:
- Low volume. Loss of water is accompanied by loss of sodium.
- Excessive sweating
- Burns
- Vomiting
- Diarrhea
- Urinary loss
- Diuretic drugs (especially thiazides)
- Addison's disease
- Cerebral salt-wasting syndrome
- Other salt-wasting kidney diseases
Treat underlying cause and give IV isotonic saline. It is important to note that sudden restoration of blood volume to normal will turn off the stimulus for continued ADH secretion. Hence, a prompt water diuresis will occur. This can cause a sudden and dramatic increase the serum sodium concentration and place the patient at risk for so-called "central pontine myelinolysis" (CPM). That disorder is characterized by major neurologic damage, often of a permanent nature.
Because of the risk of CPM, patients with low volume hyponatremia may eventually require water infusion as well as volume replacement. Doing so lessens the chance of a too rapid increase of the serum sodium level as blood volume rises and ADH levels fall.
- Normal volume.
- SIADH (syndrome of inappropriate antidiuretic hormone)
- Some cases of psychogenic polydipsia
The cornerstone of therapy for SIADH is reduction of water intake. If hyponatremia persists, then demeclocycline (an antibiotic with the side effect of inhibiting ADH) can be used. SIADH can also be treated with specific antagonists of the ADH receptors, such as conivaptan or tolvaptan.
- High volume. There is retention of water.
- Congestive heart failure
- Hypothyroidism and hypocortisolism
- Liver cirrhosis
- Nephrotic syndrome
- Psychogenic polydipsia
Placing the patient on water restriction can also help in these cases.
Severe hyponatremia may result from a few hours of heavy exercise in high temperature conditions, such as hiking in desert areas, or from endurance athletic events when electrolytes are not supplied. (Such an incident notably happened to long-distance athlete Craig Barrett in 1998).
Bovines
Sodium deficiency exists in grazing animals where soil sodium levels have been depleted by leaching. This is more common in mountainous regions. Agricultural science research conducted in the northern Thai highlands in the 1970s found that an endemic sodium deficiency masked all other nutrient deficiencies across all seasons and reduced productivity. Sodium supplementation increased liveweight gain by around 30% and also reproductive rates by around 30%. Simple salt supplementation is now recommended in this region and neighbouring mountains, as both a herd management tool and for increased productivity (see sources below).
See also
Reference
Sources
- Lindsay Falvey (1979) 'Factors Limiting Cattle Production in the Northern Thailand Highlands'. Ph.D. Dissertation, University of Queensland, Australia.
External links
amino-acids Phenylketonuria - Alkaptonuria - Ochronosis - Tyrosinemia - Maple syrup urine disease - Propionic acidemia - Methylmalonic acidemia - Isovaleric acidemia - Primary carnitine deficiency - Cystinuria - Cystinosis - Hartnup disease - Homocystinuria - Citrullinemia - Hyperammonemia - Glutaric acidemia type 1
carbohydrates Lactose intolerance - Glycogen storage disease (type I, type II, type III, type IV, type V), Fructose intolerance, Galactosemia
Lipid storage disorders Gangliosidosis - GM2 gangliosidoses (Sandhoff disease, Tay-Sachs disease) - GM1 gangliosidoses - Mucolipidosis type IV - Gaucher's disease - Niemann-Pick disease - Farber disease - Fabry's disease - Metachromatic leukodystrophy - Krabbe disease - Neuronal ceroid lipofuscinosis - Batten disease - Cerebrotendineous xanthomatosis - Wolman disease - Cholesteryl ester storage disease
List of fatty acid metabolism disorders - Hyperlipidemia - Hypercholesterolemia - Familial hypercholesterolemia - Xanthoma - Combined hyperlipidemia - Lecithin cholesterol acyltransferase deficiency - Tangier disease - Abetalipoproteinemia
mineral metabolism Disorders of calcium metabolism - Hypophosphatemia - Hypophosphatasia - Wilson's disease - Menkes disease - Hypermagnesemia - Hypomagnesemia - Hypercalcaemia - Hypocalcaemia
fluid, electrolyte and acid-base balance Electrolyte disturbance - Hypernatremia - Hyponatremia - Respiratory acidosis - Metabolic acidosis - Lactic acidosis - Hypervolemia - Hypokalemia - Hyperkalemia - Mixed disorder of acid-base balance - Hyperchloremia - Hypochloremia - Dehydration
porphyrin and bilirubin Acatalasia - Gilbert's syndrome - Crigler-Najjar syndrome - Dubin-Johnson syndrome - Rotor syndrome - Porphyria (Acute intermittent porphyria, Gunther's disease, Porphyria cutanea tarda, Erythropoietic protoporphyria, Hepatoerythropoietic porphyria, Hereditary coproporphyria, Variegate porphyria)
glycosaminoglycan Mucopolysaccharidosis - Hurler syndrome - Hunter syndrome - Sanfilippo syndrome - Morquio syndrome
glycoprotein I-cell disease - Pseudo-Hurler polydystrophy - Aspartylglucosaminuria - Fucosidosis - Alpha-mannosidosis - Sialidosis
other Alpha 1-antitrypsin deficiency - Cystic fibrosis - Familial Mediterranean fever - Lesch-Nyhan syndrome
| This page uses Creative Commons Licensed content from Wikipedia (view authors). |