mNo edit summary |
No edit summary |
||
| (26 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
| ⚫ | |||
| − | {{ClinPsy}} |
||
| ⚫ | |||
| ⚫ | * '''[[Heredity]]''' - The tendency to develop depression may be inherited; there is some evidence that this disorder may run in families. A 2004 press release from the [[National Institute of Mental Health]] declares "major depression is thought to be 40-70 percent heritable, but likely involves an interaction of several genes with environmental events." [http://depression.about.com/od/causes/a/mutantgene.htm] |
||
| − | + | ==[[Endocrinology in depression]]== |
|
| + | {{Main|Depression - Hormones}} |
||
| ⚫ | |||
| ⚫ | |||
| ⚫ | |||
| ⚫ | * '''[[Neurochemical]]''' There may be changes or imbalances in chemicals that transmit information in the brain, called [[neurotransmitters]]. Many modern [[antidepressant]] [[Psychoactive drug|drug]]s attempt to increase levels of certain [[neurotransmitters]], such as [[serotonin]] and [[norepinephrine]]. Although the causal relationship is unclear, it is known that antidepressant medications can relieve certain symptoms of depression, although critics point out that the relationship between [[serotonin]], [[SSRIs]], and depression usually is typically greatly oversimplified when presented to the public (see [http://medicine.plosjournals.org/perlserv/?request=get-document&doi=10.1371/journal.pmed.0020392 here]). |
||
| ⚫ | * '''[[Heredity]]''' - The tendency to develop [[clinical depression]] and [[depressed mood]] may be inherited; there is some evidence that this disorder may run in families. A 2004 press release from the [[National Institute of Mental Health]] declares "major depression is thought to be 40-70 percent heritable, but likely involves an interaction of several genes with environmental events." [http://depression.about.com/od/causes/a/mutantgene.htm] |
||
| ⚫ | |||
| + | |||
| ⚫ | |||
| + | |||
| + | ==[[Neuroanatomy of depression]]== |
||
*'''Neuroanatomy''' Recent research has suggested that there may be a link between depression and [[neurogenesis]] of the [[hippocampus]]. |
*'''Neuroanatomy''' Recent research has suggested that there may be a link between depression and [[neurogenesis]] of the [[hippocampus]]. |
||
| − | + | ==[[Neurochemistry of depression]]== |
|
| ⚫ | * '''[[Neurochemical]]''' There may be changes or imbalances in chemicals that transmit information in the brain, called [[neurotransmitters]]. Many modern [[antidepressant]] [[Psychoactive drug|drug]]s attempt to increase levels of certain [[neurotransmitters]], such as [[serotonin]] and [[norepinephrine]]. Although the causal relationship is unclear, it is known that antidepressant medications can relieve certain symptoms of depression, although critics point out that the relationship between [[serotonin]], [[SSRIs]], and depression usually is typically greatly oversimplified when presented to the public (see [http://medicine.plosjournals.org/perlserv/?request=get-document&doi=10.1371/journal.pmed.0020392 here]). |
||
| ⚫ | |||
| + | Most [[antidepressant]]s increase [[Chemical synapse|synaptic]] levels of [[serotonin]], one of a group of [[neurotransmitter]]s known as [[Monoamine neurotransmitter|monoamine]]s. Serotonin is thought to help regulate other neurotransmitter systems, and decreased serotonin activity may allow these systems to act in unusual and erratic ways.<ref name="IntegrativeSerotonin">{{Harvnb|Barlow|2005| p=226}}</ref> According to this "permissive hypothesis," depression can arise when low serotonin levels promote low levels of norepinephrine, another monoamine neurotransmitter.<ref>{{cite web |author=Shah N, Eisner T, Farrell M, Raeder C | year=1999 |month=July/August |url=http://www.pswi.org/professional/pharmaco/depression.pdf |title=An overview of SSRIs for the treatment of depression |work=Journal of the Pharmacy Society of Wisconsin |accessdate=2008-11-10| format=PDF}}</ref> Some antidepressants also enhance the levels of norepinephrine directly, whereas others raise the levels of [[dopamine]], a third monoamine neurotransmitter. These observations gave rise to the [[Monoamine Hypothesis|monoamine theory]] of depression. In its contemporary formulation, the monoamine theory postulates that a deficiency of certain neurotransmitters is responsible for the corresponding features of depression: "Norepinephrine may be related to alertness and energy as well as anxiety, attention, and interest in life; [lack of] serotonin to anxiety, obsessions, and compulsions; and dopamine to attention, motivation, pleasure, and reward, as well as interest in life."<ref name="pmid18494537">{{cite journal |author=Nutt DJ |title=Relationship of neurotransmitters to the symptoms of major depressive disorder |journal=Journal of Clinical Psychiatry |volume=69 Suppl E1 |pages=4–7 |year=2008 |pmid=18494537}}</ref> The proponents of this theory recommend choosing the antidepressant with the mechanism of action impacting the most prominent symptoms. Anxious and irritable patients should be treated with SSRIs or [[norepinephrine reuptake inhibitor]]s, and those experiencing a loss of energy and enjoyment of life with norepinephrine and dopamine enhancing drugs.<ref name="pmid18494537"/> |
||
| − | {{{Main|Endocrinology of depression |
||
| − | * '''[[Postpartum depression]]''' (also known as ''postnatal depression'') – Dr. Ruta M Nonacs writes that while many women experience some mood changes after giving birth, "10-15% of women experience a more disabling and persistent form of mood disturbance (eg, postpartum depression, postpartum psychosis)." [http://www.emedicine.com/med/topic3408.htm] When it occurs, the onset typically is within three months after delivery, and it may last for several months. About two new mothers out of a thousand experience the more serious depressive disorder Postnatal [[Psychosis]] which includes [[hallucination]]s and/or [[delusion]]s. |
||
| + | In the past two decades, research has uncovered multiple limitations of the monoamine theory, and its inadequacy has been criticized within the psychiatric community.<ref name="pmid10775017">{{cite journal |author=Hirschfeld RM |title=History and evolution of the monoamine hypothesis of depression |journal=Journal of Clinical Psychiatry|volume=61 Suppl 6|pages=4–6 |year=2000 |pmid=10775017}}</ref> Intensive investigation has failed to find convincing evidence of a primary dysfunction of a specific monoamine system in patients with major depressive disorders. The medications [[tianeptine]] and [[opipramol]] have long been known to have antidepressant properties despite not acting through the monoamine system. Experiments with pharmacological agents that cause depletion of monoamines have shown that this depletion does not cause depression in healthy people nor does it worsen symptoms in depressed patients.<ref name="pmid10775018">{{cite journal |author=Delgado PL |title=Depression: The case for a monoamine deficiency |journal=Journal of Clinical Psychiatry |volume=61 Suppl 6|pages=7–11 |year=2000 |pmid=10775018}}</ref> According to an essay published by the Public Library of Science, the monoamine theory, already limited, has been further oversimplified when presented to the general public.<ref name="PLoS">{{cite journal |author=Lacasse J, Leo J |title=Serotonin and depression: A disconnect between the advertisements and the scientific literature |journal=[[PLoS Medicine|PLoS Med]] |volume=2 |issue=12 |pages=e392 |year=2005 |pmid=16268734 |doi=10.1371/journal.pmed.0020392.g001|url=http://medicine.plosjournals.org/perlserv/?request=get-document&doi=10.1371/journal.pmed.0020392|accessdate=2008-10-30}}</ref> |
||
| + | |||
| + | ----- |
||
| + | |||
| + | ==See also== |
||
| + | *[[Depression - Physical treatments|physical treatments for depression]] |
||
| + | *[[Biological psychiatry]] |
||
| + | |||
| + | ==References & Bibliography== |
||
| + | <References/> |
||
| + | ==Key texts== |
||
| + | ===Books=== |
||
| + | |||
| + | ===Papers=== |
||
| + | |||
| + | ==Additional material== |
||
| + | ===Books=== |
||
| + | |||
| + | ===Papers=== |
||
| + | *[http://scholar.google.com/scholar?sourceid=mozclient&num=50&scoring=d&ie=utf-8&oe=utf-8&q=depression+biological+factors]] Google Scholar] |
||
| + | |||
| + | ==External links== |
||
| + | |||
| + | |||
| + | |||
| + | [[Category:Biological factors in mental disorders]] |
||
| + | [[Category:Depression]] |
||
| + | |||
| + | ==Physical sex differences== |
||
| + | |||
| + | {{Main|Physical sex differences and depression}} |
||
| + | |||
| + | ==Medical conditions and depression== |
||
* '''Medical conditions''' – Certain illnesses, including cardiovascular disease<ref>{{cite journal | url = http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=15581413&query_hl=7 | title = 5-Lipoxygenase as a putative link between cardiovascular and psychiatric disorders | last = Manev | first = R | coauthors = Manev H | journal = Critical Reviews in Neurobiology | date = 2004 | volume = 16 | issue = 1�2 | pages = 181�6 }}</ref>, [[hepatitis]], [[mononucleosis]], [[hypothyroidism]], and organic brain damage caused by degenerative conditions such as Parkinson disease or by traumatic blunt force injury may contribute to depression, as may certain prescription drugs such as [[oral contraceptive|birth control pills]] and [[steroid]]s. Gender dysphoria can also cause depression. |
* '''Medical conditions''' – Certain illnesses, including cardiovascular disease<ref>{{cite journal | url = http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=pubmed&dopt=Abstract&list_uids=15581413&query_hl=7 | title = 5-Lipoxygenase as a putative link between cardiovascular and psychiatric disorders | last = Manev | first = R | coauthors = Manev H | journal = Critical Reviews in Neurobiology | date = 2004 | volume = 16 | issue = 1�2 | pages = 181�6 }}</ref>, [[hepatitis]], [[mononucleosis]], [[hypothyroidism]], and organic brain damage caused by degenerative conditions such as Parkinson disease or by traumatic blunt force injury may contribute to depression, as may certain prescription drugs such as [[oral contraceptive|birth control pills]] and [[steroid]]s. Gender dysphoria can also cause depression. |
||
| + | |||
{{Main|Depression and physical illness}} |
{{Main|Depression and physical illness}} |
||
| + | ==Physiological functioning and depression== |
||
| − | * '''Nutrition''' – The increase in depression in industrialised societies has been linked to [[diet]], particularly to reduced levels of [[omega-3]] [[fatty acids]] in [[intensive farming|intensively farmed]] food and processed foods<ref>{{cite book | first = Felicity | last = Lawrence | year = 2004 | title = Not on the Label | chapter = The Ready Meal | editor = Kate Barker | pages = 214 | publisher = Penguin | id = ISBN 0-141-01566-7 }}</ref>. This link has been at least partly validated by studies using [[dietary supplements]] in schools<ref>{{cite web | title = Using Fatty Acids for Enhancing Classroom Achievement | url = http://www.durhamtrial.org/ | accessdate = January | accessyear = 2004 }}</ref> and by a double-blind test in a prison. An excess of [[omega-6]] [[fatty acids]] in the diet was shown to cause depression in [[rats]]<ref>{{cite web | title = Omega-6 Levels in Brain Linked to Depression | url = http://www.fishoilblog.com/benefits/omega-6-levels-in-brain-linked-to-depression.php | accessdate = May | accessyear = 2006 }}</ref>. |
||
| + | The activity of various physiological processes are also associated with depression: |
||
| + | |||
| + | *[[Depression, sleep and the circadian rhythm]] |
||
| + | |||
| + | ==Nutrition and depression== |
||
| + | *The increase in depression in industrialised societies has been linked to [[diet]], particularly to reduced levels of [[omega-3]] [[fatty acids]] in [[intensive farming|intensively farmed]] food and processed foods. |
||
{{Main|Nutrition and depression}} |
{{Main|Nutrition and depression}} |
||
| + | ==Drug abuse and depression== |
||
| − | * '''Alcohol and other drugs''' – Alcohol can have a negative effect on mood, and misuse of alcohol, [[benzodiazepine]]-based tranquilizers, and sleeping medications can all play a major role in the length and severity of depression. The link between frequent [[cannabis]] use and depression is also widely documented, although the direction of causality remains in question; Dr. Salynn Boyles writes, "...research has linked pot smoking with depression and schizophrenia ... daily use [of [[marijuana]]] was associated with a five-fold increase in later depression and anxiety among young women. But depression and anxiety were not predictive of later [[marijuana use]]." [http://www.webmd.com/content/article/53/61380.htm?z=1728_00000_1000_ln_01] |
||
| + | * '''Alcohol and other drugs''' – Alcohol can have a negative effect on mood, and misuse of alcohol, benzodiazepine-based tranquilizers, sleeping medications and recreational drugs can all play a major role in the length and severity of depression. |
||
| + | |||
| ⚫ | |||
| + | |||
| + | ==See also== |
||
| + | |||
| + | ==Bibliography== |
||
| + | |||
| + | ===Key texts – Books=== |
||
| + | |||
| + | ===Additional material – Books=== |
||
| + | |||
| + | ===Key texts – Papers=== |
||
| + | <References/> |
||
| + | |||
| + | ===Additional material - Papers=== |
||
| + | *[http://scholar.google.com/scholar?sourceid=mozclient&num=50&scoring=d&ie=utf-8&oe=utf-8&q=Depression+biological+factors Google Scholar] |
||
| + | |||
| + | ==External links== |
||
| + | |||
| + | |||
| + | [[Category:Biological factors in depression]] |
||
| + | [[Category:Depression]] |
||
| + | {{Depression}} |
||
| ⚫ | |||
| − | [[Link title]] |
||
Latest revision as of 17:22, 25 March 2010
Biological causes
Endocrinology in depression
- Main article: Depression - Hormones
- Hormonal factorsThe levels of hormones, the chemical messengers in the body that help regulate metabolism, have been linked to depression
Genetic factors in depression
- Heredity - The tendency to develop clinical depression and depressed mood may be inherited; there is some evidence that this disorder may run in families. A 2004 press release from the National Institute of Mental Health declares "major depression is thought to be 40-70 percent heritable, but likely involves an interaction of several genes with environmental events." [1]
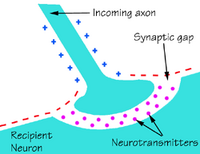
Brain chemicals called neurotransmitters allow electrical signals to move from the axon of one nerve cell to the neuron of another. A shortage of neurotransmitters impairs brain communication.
Neuroanatomy of depression
- Neuroanatomy Recent research has suggested that there may be a link between depression and neurogenesis of the hippocampus.
Neurochemistry of depression
- Neurochemical There may be changes or imbalances in chemicals that transmit information in the brain, called neurotransmitters. Many modern antidepressant drugs attempt to increase levels of certain neurotransmitters, such as serotonin and norepinephrine. Although the causal relationship is unclear, it is known that antidepressant medications can relieve certain symptoms of depression, although critics point out that the relationship between serotonin, SSRIs, and depression usually is typically greatly oversimplified when presented to the public (see here).
Most antidepressants increase synaptic levels of serotonin, one of a group of neurotransmitters known as monoamines. Serotonin is thought to help regulate other neurotransmitter systems, and decreased serotonin activity may allow these systems to act in unusual and erratic ways.[1] According to this "permissive hypothesis," depression can arise when low serotonin levels promote low levels of norepinephrine, another monoamine neurotransmitter.[2] Some antidepressants also enhance the levels of norepinephrine directly, whereas others raise the levels of dopamine, a third monoamine neurotransmitter. These observations gave rise to the monoamine theory of depression. In its contemporary formulation, the monoamine theory postulates that a deficiency of certain neurotransmitters is responsible for the corresponding features of depression: "Norepinephrine may be related to alertness and energy as well as anxiety, attention, and interest in life; [lack of] serotonin to anxiety, obsessions, and compulsions; and dopamine to attention, motivation, pleasure, and reward, as well as interest in life."[3] The proponents of this theory recommend choosing the antidepressant with the mechanism of action impacting the most prominent symptoms. Anxious and irritable patients should be treated with SSRIs or norepinephrine reuptake inhibitors, and those experiencing a loss of energy and enjoyment of life with norepinephrine and dopamine enhancing drugs.[3]
In the past two decades, research has uncovered multiple limitations of the monoamine theory, and its inadequacy has been criticized within the psychiatric community.[4] Intensive investigation has failed to find convincing evidence of a primary dysfunction of a specific monoamine system in patients with major depressive disorders. The medications tianeptine and opipramol have long been known to have antidepressant properties despite not acting through the monoamine system. Experiments with pharmacological agents that cause depletion of monoamines have shown that this depletion does not cause depression in healthy people nor does it worsen symptoms in depressed patients.[5] According to an essay published by the Public Library of Science, the monoamine theory, already limited, has been further oversimplified when presented to the general public.[6]
See also
- physical treatments for depression
- Biological psychiatry
References & Bibliography
- ↑ Barlow 2005, p. 226
- ↑ Shah N, Eisner T, Farrell M, Raeder C (1999). An overview of SSRIs for the treatment of depression. (PDF) Journal of the Pharmacy Society of Wisconsin. URL accessed on 2008-11-10.
- ↑ 3.0 3.1 Nutt DJ (2008). Relationship of neurotransmitters to the symptoms of major depressive disorder. Journal of Clinical Psychiatry 69 Suppl E1: 4–7.
- ↑ Hirschfeld RM (2000). History and evolution of the monoamine hypothesis of depression. Journal of Clinical Psychiatry 61 Suppl 6: 4–6.
- ↑ Delgado PL (2000). Depression: The case for a monoamine deficiency. Journal of Clinical Psychiatry 61 Suppl 6: 7–11.
- ↑ Lacasse J, Leo J (2005). Serotonin and depression: A disconnect between the advertisements and the scientific literature. PLoS Med 2 (12): e392.
Key texts
Books
Papers
Additional material
Books
Papers
- [2]] Google Scholar]
External links
Physical sex differences
- Main article: Physical sex differences and depression
Medical conditions and depression
- Medical conditions – Certain illnesses, including cardiovascular disease[1], hepatitis, mononucleosis, hypothyroidism, and organic brain damage caused by degenerative conditions such as Parkinson disease or by traumatic blunt force injury may contribute to depression, as may certain prescription drugs such as birth control pills and steroids. Gender dysphoria can also cause depression.
- Main article: Depression and physical illness
Physiological functioning and depression
The activity of various physiological processes are also associated with depression:
- Depression, sleep and the circadian rhythm
Nutrition and depression
- The increase in depression in industrialised societies has been linked to diet, particularly to reduced levels of omega-3 fatty acids in intensively farmed food and processed foods.
- Main article: Nutrition and depression
Drug abuse and depression
- Alcohol and other drugs – Alcohol can have a negative effect on mood, and misuse of alcohol, benzodiazepine-based tranquilizers, sleeping medications and recreational drugs can all play a major role in the length and severity of depression.
- Main article: Drug abuse and depression
See also
Bibliography
Key texts – Books
Additional material – Books
Key texts – Papers
- ↑ Manev, R, Manev H (2004). 5-Lipoxygenase as a putative link between cardiovascular and psychiatric disorders. Critical Reviews in Neurobiology 16 (1�2): 181�6.
Additional material - Papers
External links